Ultrasound Mapping in Injectables
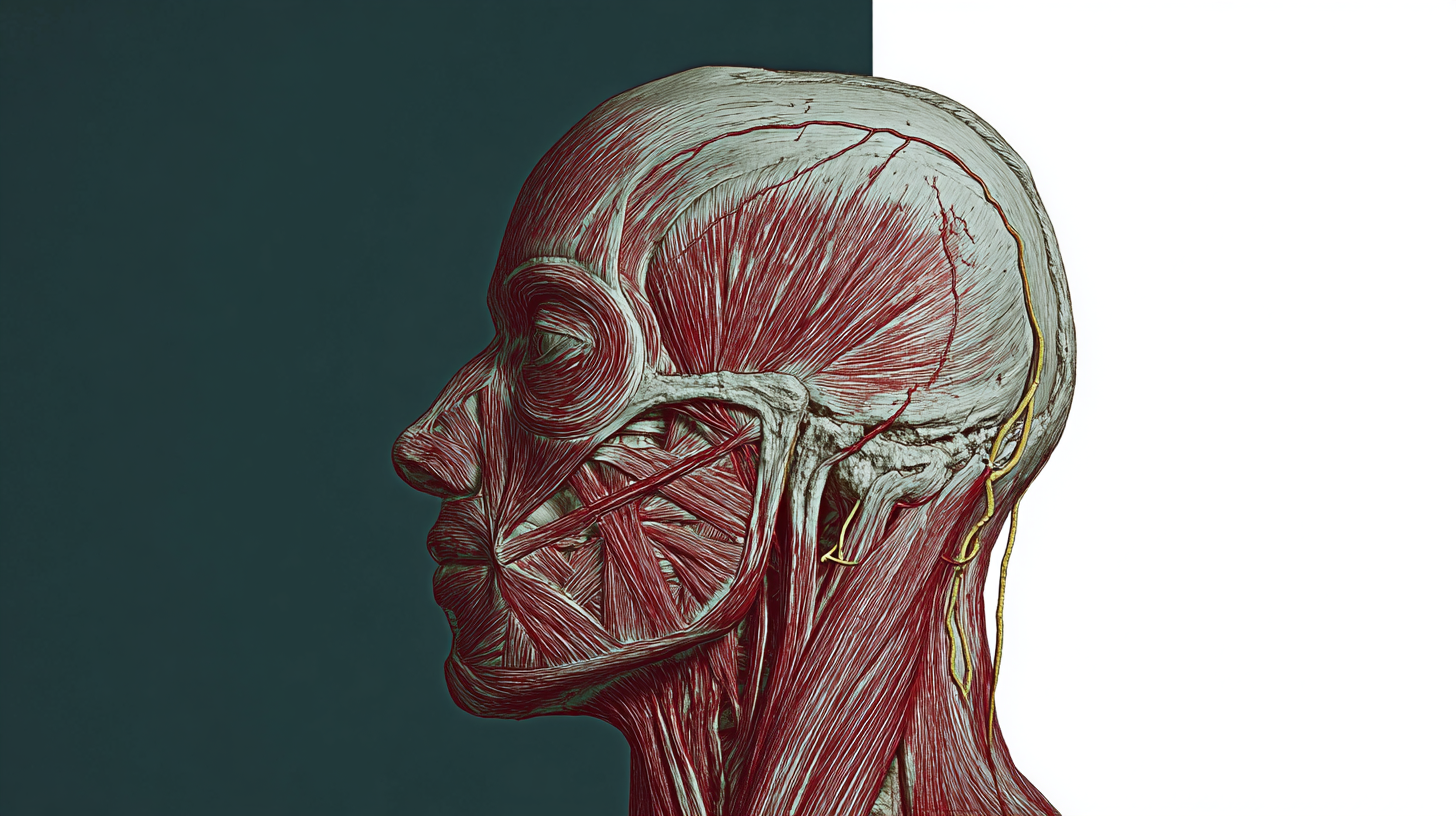
Point of care ultrasound is moving from emergency rooms into aesthetic clinics, where it is being used to map vessels, confirm injection planes and troubleshoot complications in real time. High frequency probes can visualise superficial soft tissue with impressive detail, so practitioners can plan, inject and document with far greater confidence than with palpation alone. Early studies and expert guidance suggest that ultrasound guidance lowers risk and improves placement accuracy, particularly in high stakes areas like the midface and temples.
What ultrasound adds, in practice
A high frequency linear probe, ideally 15 to 20 MHz, resolves the epidermis, dermis, fat compartments and fascial layers. Switch on colour or power Doppler and moving blood reveals arterial and venous structures to avoid. Operators can follow the cannula tip in plane, confirm the depth of the target compartment and capture evidence of where product sits after each pass. In the upper face and midface this combination of grey scale and Doppler improves the accuracy of placement and reduces the chance of intravascular injection or compression.
Midface mapping, step by step
Begin with a light sweep over the nasolabial and medial cheek to identify the facial artery as it ascends towards the angular artery. Use Doppler to track flow where the vessel courses close to typical injection routes, then mark its path before you begin. Scan across the infraorbital region to locate the infraorbital foramen and accompanying artery and vein, which often align near the mid-pupillary line; a brief Doppler check helps distinguish vessel types and depth. This pre-map takes minutes and reduces guesswork when working in tear trough, lid-cheek junction and medial cheek. In live guidance, track the cannula in plane and confirm the intended layer, for example supraperiosteal bolus versus superficial fat threads, then verify product location on a quick post-scan.
Temple work, where ultrasound changes the game
Temple hollowing is popular yet unforgiving because vessels and nerves run in variable positions and the fat layers are thin. Ultrasound can show the superficial temporal artery and its frontal branch, the sentinel vein and the deep temporal fascia, so you can select a plane and route that avoids them. Many clinicians either place small volumes deep on periosteum or stay very superficial with a cannula in the subdermal layer, choices that become more defensible when the artery has been mapped first. Real time Doppler confirms distance from the vessel during injection and a post-injection scan can evidence the depot or line of filler. Recent anatomical reviews reinforce the value of identifying planes and key structures before treating the temple.
Facial vasculature is notoriously variable. Anatomy texts offer averages, not certainties, so imaging augments anatomy rather than replaces it. The most robust message from complication literature is that every area can be hazardous, which is precisely why vessel mapping and plane confirmation are worth the extra minutes.
Complication prevention and management
Early ultrasound can help recognise vascular events by revealing intraluminal filler, external vessel compression or downstream perfusion changes. In suspected occlusion, ultrasound guidance allows targeted hyaluronidase around the embolus or compressive bolus and helps the clinician monitor tissue reperfusion as care proceeds. Case series and guidelines document successful ultrasound-guided dissolving for hyaluronic acid fillers, with dosing adjusted to clot size and location. Ultrasound is equally useful later on to locate and treat delayed nodules or misplaced product.
Building POCUS into clinic workflow
Adopt a simple three-moment rhythm. First, pre-map in two to three minutes per side, mark key vessels and confirm the target plane. Second, use live guidance for the riskiest passes so you can see the cannula tip and maintain separation from vessels. Third, post-scan to confirm product depth and create a visual record for the notes. Store stills or short clips with depth annotations and Doppler settings, which strengthens consent and supports audit. As skills grow, many teams reserve live guidance for the highest risk zones or revision work, while using pre- and post-scans for routine cheeks and temples.
Training, devices and caveats
Choose a portable system that offers at least 15 MHz with sensitive colour or power Doppler and a small footprint linear probe that fits the temple and tear trough comfortably. Hygiene matters: use sterile gel for any passes that approach injection sites and follow local infection control policies. Expect a learning curve, especially when distinguishing arteries from veins. Gentle probe pressure can collapse veins and hide flow, so reduce pressure and adjust Doppler scale to avoid false reassurance. Not every artery will be visible in every patient and artefacts are common until the operator gains experience, which is why ultrasound should be paired with robust anatomical knowledge and conservative dosing.
The value proposition is simple. Imaging turns a blind procedure into one that is planned and documented. It helps clinicians avoid vessels in areas where variation is the rule, supports accurate placement in defined tissue planes and gives a rapid pathway for diagnosing and treating complications if they occur. For the midface and temples, where aesthetics and risk intersect, ultrasound is fast becoming a practical standard that raises both safety and trust.